| Medical Device | Requirement | Drug |
|---|---|---|
| CDRH Center for Devices and Radiological Health is responsible for protecting and promoting the public health by assuring that patients and providers have timely and continued access to safe, effective, and high-quality medical devices and safe radiation-emitting products | Center | CDER Center for Drug Evaluation and Research regulates human drugs. If the primary intended use of the product is achieved through chemical action or by being metabolized by the body, the product may be considered a drug. |
|
An instrument, apparatus, implement, machine, contrivance, implant, in vitro reagent, or other similar or related article, including a component part, or accessory which is: (A) recognized in the official National Formulary, or the United States Pharmacopoeia, or any supplement to them, (B) intended for use in the diagnosis of disease or other conditions, or in the cure, mitigation, treatment, or prevention of disease, in man or other animals, or (C) intended to affect the structure or any function of the body of man or other animals, and which does not achieve its primary intended purposes through chemical action within or on the body of man or other animals and which is not dependent upon being metabolized for the achievement of its primary intended purposes. The term "device" does not include software functions excluded pursuant to section 520(o). |
Definition |
A substance recognized by an official pharmacopeia or formulary. A substance intended for use in the diagnosis, cure, mitigation, treatment, or prevention of disease. A substance (other than food) intended to affect the structure or any function of the body. A substance intended for use as a component of a medicine but not a device or a component, part or accessory of a device. |
| Band aids, Syringes, Ventilators, Pacemaker, Breast Implant | Examples | Pizensy, Tazverik, Tepezza, Ayvakit |
| Class I, Class II, Class III | Classification | Prescription drugs, Over the counter drugs (OTC) |
| Medical Device: 800 - 898, Mammography Quality Std Act: 900, Radiological Health: 1000 - 1040 | 21 CFR Parts | Drugs General: 200 -299, Drugs for Human Use: 300 - 499 |
| For new Medical Device: 3 to 7 years | Total Timeline to Enter Market | For new Drug - 10 to 12 years |
| Class I: Exempt or 510(k), Class II: 510(k), DeNovo or PMA, Class III: PMA/DeNovo/HDE | Regulatory Pathway for Submissions | Traditional NDA: 505 (b) (1), Hybrid NDA: 505(b)(2), ANDA: 505 (j) generics, NDA Supplement |
|
Substantial Equivalence: It means that the new device is as safe and effective as the predicate. A device is substantially equivalent if, in comparison to a predicate it: ● has the same intended use as the predicate; and ● has the same or different technological characteristics as the predicate but it does not raise different questions of safety and effectiveness; Reference device: It is a legally marketed device that is used to provide scientific or technical information to help address the safety and effectiveness of a new technological characteristic Humanitarian device exemption (HDE): It is one that is expected to treat or diagnose conditions that affect fewer than 4,000 individuals in the United States annually. HDE are handled through the Office of Orphan Products Development at the FDA
|
Terms |
Generic Drug: A generic drug is a medication created to be the same as an already marketed brand-name drug in dosage form, safety, strength, route of administration, quality, performance characteristics, and intended use. These similarities help to demonstrate bioequivalence, which means that a generic medicine works in the same way and provides the same clinical benefit as the brand-name medicine. In other words, you can take a generic medicine as an equal substitute for its brand-name counterpart. Innovator Drug or Reference Productor RLD A reference product is the single biological product, already approved by FDA, against which a proposed biosimilar product is compared or A Reference Listed Drug (RLD) is an approved drug product to which new generic versions are compared to show that they are bioequivalent. Orphan Drugs: As a drug intended to treat a condition affecting fewer than 200,000 persons in the United States, or which will not be profitable within 7 years following approval by the FDA |
|
510k types Traditional 510(k) is used for any original device that has not been previously cleared and is not required to go through the PMA process. The Traditional 510(k) is also used for a change to a previously cleared device that does not qualify for a Special 510(k). Special 510(k) is for medical devices that are already cleared under a Traditional 510(k) and have had significant changes made so that they need to go through clearance again Abbreviated 510(k) is used when device manufacturers may choose to submit this type of 510(k) when the submission relies on: FDA guidance document(s), Demonstration of compliance with special control(s) for the device type, or Voluntary consensus standard(s). |
Types of Pathway |
NDA pathway Types The 505(b)(1) is a US FDA Regulatory pathway used to obtain approval for new drugs with previously unapproved active ingredients. The 505(b)(2) is the US FDA Regulatory pathway for approving a new drug which has previously approved active ingredients. 505j application is an abbreviated new drug application (ANDA) that contains the information to show that the proposed product is identical in active ingredient , dosage form , strength, route of administration, labeling, quantity,performance characteristics and intended use , among other things , to previously approved product-the reference listed drug RLD. An NDA supplement is an application to allow a company to make changes in a product that already has an approved new drug application (NDA). |
|
Ecopy (electronic copy) for PMA eSTAR (electronic Submission Template and Resource) for 510k |
Document Submission method | eCTD: electronic Common Technical Document |
| The Device Development Process Step 1: Device Discovery and Concept Step 2: Preclinical Research- Prototype Step 3: Pathway to Approval Step 4: FDA Device Review Step 5: FDA Post- Market Device Safety Monitoring | Development Process | The Drug Development Process Step 1 Discovery and Development Step 2 Preclinical Research Step 3 Clinical Research Step 4 FDA Review Step 5 FDA Post-Market Safety Monitoring |
| 21 CFR 803.20 | PMS | 21 CFR 314.80 |
| An investigational device exemption (IDE) allows the investigational device to be used in a clinical study in order to collect safety and effectiveness data. Clinical studies are most often conducted to support a PMA. | To Perform Clinical Trials |
An Investigational New Drug Application (IND) is a request from a clinical study sponsor to obtain authorization from the FDA to administer an investigational drug or biological product to humans. Clinical studies are often conducted to collect safety and effectiveness information in support of marketing applications for biologic and drug products. |
| The Medical Device Reporting (MDR) regulation (21 CFR Part 803) contains mandatory requirements for manufacturers, importers, and device user facilities to report certain device-related adverse events and product problems to the FDA. Manufacturers: Manufacturers are required to report to the FDA when they learn that any of their devices may have caused or contributed to a death or serious injury. Manufacturers must also report to the FDA when they become aware that their device has malfunctioned and would be likely to cause or contribute to a death or serious injury if the malfunction were to recur. |
Adverse Event Reporting | The Adverse Event Reporting System (AERS) is a computerized information database designed to support the FDA's post-marketing safety surveillance program for all approved drug and therapeutic biologic products. The FDA uses AERS to monitor for new adverse events and medication errors that might occur with these marketed products. Reporting of adverse events from the point of care is voluntary in the United States. FDA receives some adverse event and medication error reports directly from health care professionals (such as physicians, pharmacists, nurses and others) and consumers (such as patients, family members, lawyers and others). Healthcare professionals and consumers may also report these events to the products' manufacturers. If a manufacturer receives an adverse event report, it is required to send the report to FDA as specified by regulations. |
|
5, 10 , 30 days depending on the hazard. Manufacturers must report regarding death or serious injury within 30 days of the event and Must report in case of device malfunction within 30 days of the event |
Adverse Event Report Timeline | IND safety report” for 15-day reports, or “7-day IND safety report” for unexpected fatal or life-threatening suspected adverse reaction reports, or |
| Medical Device Quality System Regulation (QSR), 21 CFR part 820 | cGMP Regulations | |
| Medical Device Databases A listing of databases on a variety of topics of interest for CDRH Stakeholders | Database | Drug Approvals and Databases A listing of databases on a variety of topics of interest for CDER Stakeholders |
| MDUFA Medical Device User Fee Amendments is a set of agreements between the Food and Drug Administration (FDA) and the medical device industry to provide funds for the Office of Device Evaluations (ODE) to review medical device submissions. | User fee | PDUFA Prescription Drug User Fee Act was created by Congress in 1992 and authorizes FDA to collect user fees from persons that submit certain human drug applications for review or that are named in approved applications as the sponsor of certain prescription drug products. |
| Requests for Feedback and Meetings for Medical Device Submissions: The Q-Submission Program | Types of FDA Formal Meetings | Formal Meetings between the FDA and Sponsors or Applicants of PDUFA Products Guidance for Industry |
|
FDA action on a 510k takes 90 calendar days from the day of 510k received and the date of the decision excluding the hold dates FDA action on a PMA takes within 180 days of the date of filling of the PMA |
Timeline for Review by FDA |
Once the FDA receives an NDA, the review team decides if it is complete. If it is not complete, the review team can refuse to file the NDA. If it is complete, the review team has 6 to 10 months to make a decision on whether to approve the drug. Once the IND is submitted, the sponsor must wait 30 calendar days before initiating any clinical trials. FDA shall approve or disapprove the ANDA application within 180 days of the initial receipt of an application FDA promulgated regulations |
|
Phase 1: Pilot / Early Feasibility n = 10 to 40 Phase 2: Feasibility n = 50 to 100 Phase 3: Pivotal n = several 100's Phase 4: Post Market n = several 1000's |
Clinical Trial Phases |
Phase 1: Safety & Toxicity n = 10 to 80 Phase 2: Safety & Efficacy n = 100's Phase 3: Clinical Effectiveness n = 100 - 1000's Phase 4: Post Market n = 1000's |
| ISO 13485, ISO 9001 | ISO Standards | ISO 9001, ICH guidelines, WHO GMP guidelines |
| FORM FDA 3514: CDRH PREMARKET REVIEW SUBMISSION COVER SHEET | Forms | Form 0356h: Application to Market a New or Abbreviated New Drug or Biologic for Human Use |
| ISO 14155 : Clinical investigation of medical devices for human subjects | Adverse Events in Clinical trials | ICH E6(R2) Good Clinical Practice: Adverse Drug Reaction |
|
Verification: Did I make the product right? Validation: Did I make the right product? |
Common Terms |
Pharmacokinetics: What the body does to the drug? Pharmacodynamics: What the drug does to the body? |
|
The FDA is authorized to regulate the advertising of restricted medical devices; 21 U.S.C. B' 352(r) provides that a restricted device is misbranded if its advertising does not contain a brief statement of the device's intended use and relevant warnings, precautions, side effects and contraindications. |
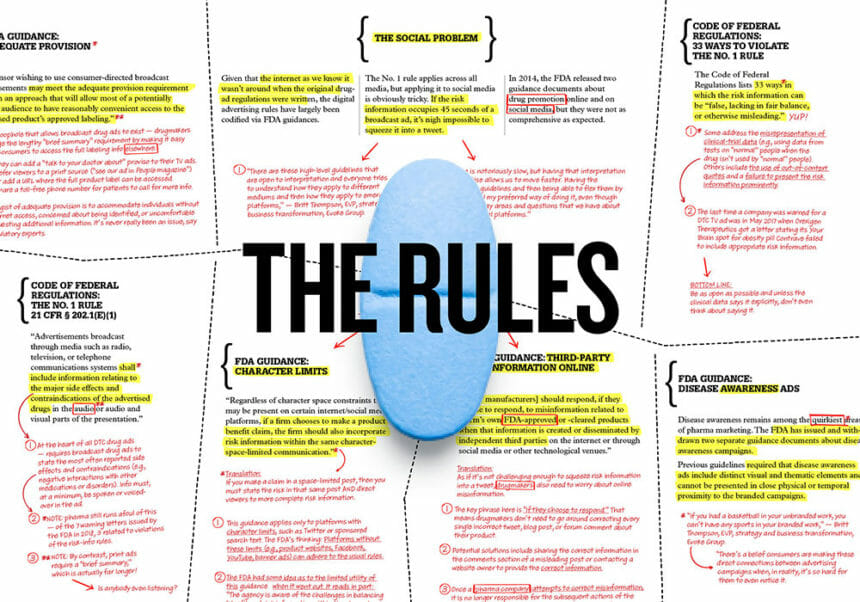
Advertising or Promotion | The FDA drug advertising regulations require that advertisements for prescription drugs only promote them for medical uses that have been evaluated and approved by the agency. In addition, the ads must present a fair balance between the benefits and risks. OPDP (The Office of Prescription Drug Promotion) protects the public health by helping to ensure that prescription drug promotion is truthful, balanced, and accurately communicated. The FDA does not oversee the advertising of over-the-counter (OTC) drugs. The Federal Trade Commission (FTC) is responsible for regulating OTC drug ads |
|
Premarket Requirements for medical device: Step One: Classify Your Device and Understand Applicable Regulatory Controls Step Two: Select and Prepare the Correct Premarket Submission Step Three: Send your Premarket Submission to the FDA and Interact with FDA Staff During Review Step Four: Comply with Applicable Regulatory Controls Including the Establishment Registration and Device Listing |
Miscellaneous Requirements |
FDA Drug Review process
Preclinical (animal) testing. An investigational new drug application (IND) outlines what the sponsor of a new drug proposes for human testing in clinical trials. Phase 1 studies (20 to 80 people). Phase 2 studies (a few dozen to 300 people). Phase 3 studies (several 100 to 3,000 people). The pre-NDA period, just before a new drug application (NDA) is submitted. A common time for the FDA and drug sponsors to meet. Submission of an NDA is the formal step asking the FDA to consider a drug for marketing approval. After an NDA is received, the FDA has 60 days to decide whether to file it so it can be reviewed. If the FDA files the NDA, an FDA review team is assigned to evaluate the sponsor's research on the drug's safety and effectiveness. The FDA reviews information that goes on a drug's professional labeling (information on how to use the drug). The FDA inspects the facilities where the drug will be manufactured as part of the approval process. FDA reviewers will approve the application or issue a complete response letter. |
| Medical Device Information: 301–796–5733. | Contact Number | Drug Information: 301-796-3400 |
The distinction between medical devices and drugs is fundamental yet often misunderstood. While both serve critical roles in patient care, their regulatory pathways diverge significantly, shaping the development, approval, and marketing processes for manufacturers. Understanding the nuances of regulatory oversight by the US Food and Drug Administration (FDA) is paramount for companies seeking to bring innovative healthcare solutions to market.
This article aims the intricate regulatory framework that governs medical devices and drugs under US FDA oversight. By highlighting key distinctions and regulatory requirements, such as FDA centers, classification, pathways, submission protocols, and development processes, readers gain invaluable insights into the nuanced differences between these biomedical products. From navigating clinical trials to managing adverse events and adhering to strict timelines, understanding the regulatory criteria for each product type is essential for ensuring compliance and patient safety. Moreover, this article provides direct links to FDA resources, empowering readers to delve deeper into specific regulatory topics. With clear and concise information at their fingertips, healthcare professionals, manufacturers, and regulatory experts can confidently navigate the complex terrain of FDA regulations, fostering innovation while upholding the highest standards of quality and safety.
Author.: Akash Kirani
Tags
US FDA